Category Archives: Heart Disease
Supplements as Part of a Heart-Healthy Regimen

Supplementation has become an ever-greater part of the collective psyche in the US. As dietary and lifestyle habits have changed, and more of us suffer from metabolic diseases due to excess weight, our understanding of bodily functions and vitamin and mineral interactions has improved. Are we on the right track, or have we taken it too far? Today, you can’t go to a big box store without seeing rows of supplements, from those we know well to obscure roots and herbs that we have difficulty pronouncing. With all the claims swirling around each of these supplements, do they have a place in maintaining cardiovascular health, or do they represent a Band-Aid for those looking for an easy way out? Continue reading →
When You May Need Early Heart Health Screening
When you’re young and healthy, the last thing on your mind is keeping up with heart screenings. It may seem like a distant problem that you will not have to deal with for many years to come. But the truth is that the more proactive you are about your heart health, the better chance you have of detecting a condition early, opening up widerpossibilities for prevention and treatment.
Just as women perform self-breast exams, men get prostate checks and we are all recommended to get colonoscopies at certain ages, regular heart screenings are imperative for your health and well-being.
Does Pollution Affect Heart Health?
As we become more aware of the impact we have on the environment, the conversation about air pollution is ever more important. The pollutants released into the air not only have a negative impact on the environment. It is something you are exposed to every day, but you may be surprised by the effects – both short and long term – that pollution has on your heart and heart health.
Does Walking Improve Cardiovascular Health?
It may seem like a very basic solution to the number one killer in the United States and many countries around the world. However, walking offers a number of incredible benefits that can help reverse cardiovascular risk and stop further degradation of heart health. Unfortunately, inactivity and a sedentary lifestyle – which has become all too common in American life these days – has only increased the incidence of severity of heart disease. And while many patients with cardiovascular issues embark on significant, drastic diet and exercise programs, they are usually unsustainable and often the underlying issues such as obesity are not resolved – sometimes they’re even worsened.
New Research on High Blood Pressure and The Risk of Cognitive Decline
There has been quite a bit of discussion about cardiovascular health and its association with cognitive decline, including dementia of which Alzheimer’s is the most common form. Unfortunately, it seems that as our collective societal health has worsened over the years – generally through poor dietary and exercise habits – so too has the outlook for cognitive impairment in our later years. Research has shown that cognitive decline can be hastened by long-term heightened blood pressure problems known as hypertension. However, a recent study has shed more light on this phenomenon and shown that even short bouts of elevated high blood pressure can bring on cognitive decline more rapidly. This latest study was performed in Brazil on over 7000 adults averaging around 59 years of age. These adults were followed for four years and tested for memory and other cognitive function. It was found that untreated high blood pressure was associated with cognitive decline. This was true even for a pre-hypertension – elevated blood pressure that does not qualify as true hypertension.
This latest study was performed in Brazil on over 7000 adults averaging around 59 years of age. These adults were followed for four years and tested for memory and other cognitive function. It was found that untreated high blood pressure was associated with cognitive decline. This was true even for a pre-hypertension – elevated blood pressure that does not qualify as true hypertension.
Obesity and How It Affects The Heart
Your Weight and Heart Health
Obesity is linked to increased risk for developing cardiovascular disease including heart failure, arrythmia and coronary heart disease. Clinically, a healthy weight is defined by a body mass index between 18.5 and 24.9. Overweight is marked at BMI 25 to 29.9 and obese is 30 and above. You can figure out your BMI using a BMI calculator or checking your stats in your patient portal from recent visits.
NSAIDs and Risks for Your Heart
NSAIDs, used to treat pain and inflammation, can increase your risk for both stroke and heart attack. The FDA has warned about this increased risk since the early 2000s. However, taking a non-steroidal anti-inflammatory medication to treat a specific ailment for a short period of time should not create an extreme risk. Extended use can be dangerous, so we recommended that you take the smallest amount necessary for the shortest period of time possible.
Stress Can Affect the Heart, But Not How You May Think
For many decades, it was believed that stress in and of itself caused heart disease and an increased risk of heart attack. Stress, in fact, has been linked to a number of diseases and disorders and has even been proven to increase the severity of some disorders.
How to Know It’s Time to Visit Your Cardiologist
Many of us wait until our symptoms are obvious and even debilitating before we seek medical help. This can also be true with cardiovascular issues. Many times, shrugging off smaller abnormalities leads to progressively worse symptoms and ultimately an unfavorable diagnosis with fewer treatment options. With high cholesterol and high blood pressure issues becoming more and more prevalent in the United States the old thinking that heart disease only affects to the elderly is no longer true.
In fact, prevention starts at a young age. 30, 40 and 50-year-olds that address their risk of heart disease, can add years to their life and avoid serious complications later on.
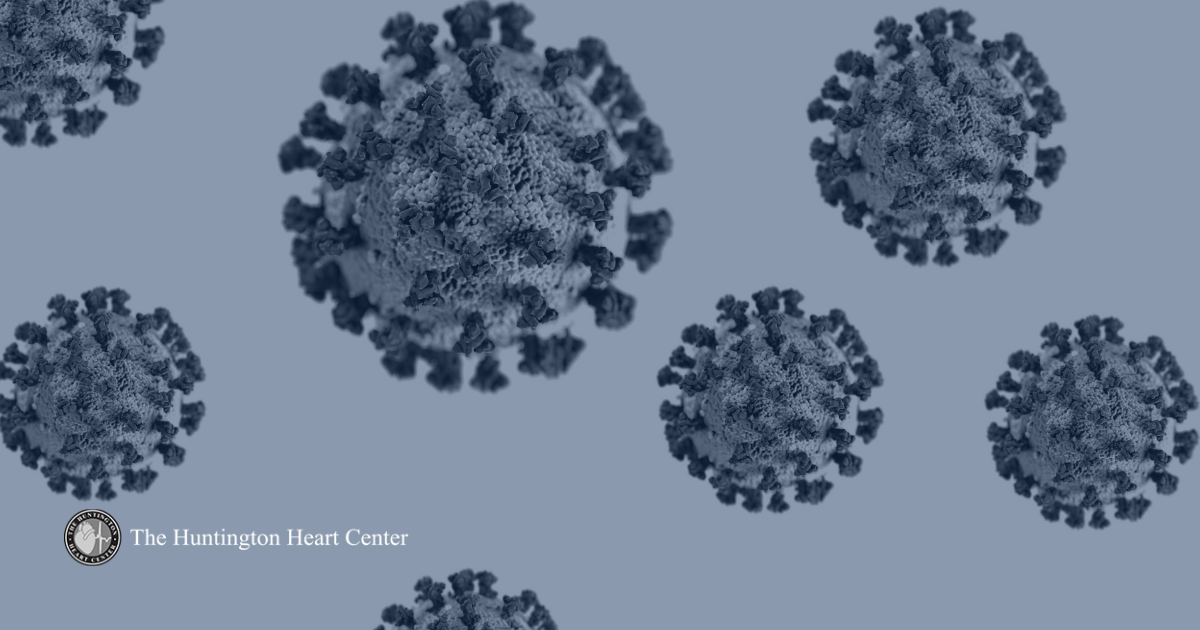
Lasting Heart Disease and COVID-19
While New York has seen a precipitous drop in COVID-19 cases and deaths after our devastating first wave, we are certainly not out of the woods. There’s a lot we don’t know, both about the disease itself and about how transmissible it currently is and will be in the fall, when everyone expects a second wave.
Adding to this uncertainty is recent research from Germany which shows many patients, especially those with severe COVID infections may have long lasting heart defects and injury along with other medical deficits including neurological issues and lung problems.